Image
By late January 2026, public health officials are confronting a flu season that refuses to follow a familiar script. After a deceptively quiet fall, influenza activity surged sharply in mid-to-late December and has continued to drive hospitalizations and deaths across the country. In Minnesota and much of the Midwest, the worst may still be ahead.
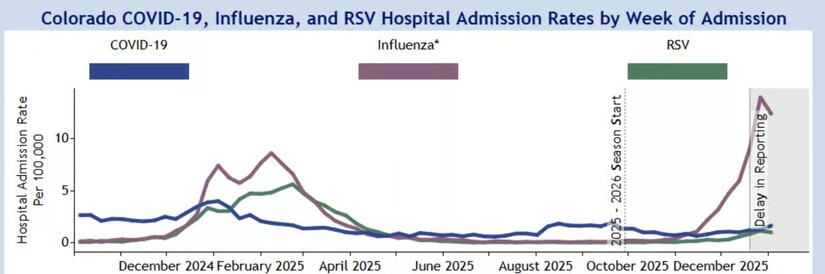
State and federal surveillance data show a season marked by rapid acceleration, high severity among vulnerable populations, and the dominance of a particularly aggressive strain of Influenza A. While some regions have reported brief signs of stabilization, health authorities caution that the 2025–2026 flu season has not yet peaked in many states.

According to the Minnesota Department of Health (MDH), influenza-related hospitalizations and deaths have climbed steadily through January. The most recent weekly surveillance reports document thousands of hospital admissions, more than 100 adult flu-associated deaths, and widespread outbreaks in schools and long-term care facilities across the state.
Laboratory testing shows a persistently high share of positive flu results, a signal of broad community spread rather than isolated outbreaks. MDH officials note that severe outcomes such as hospitalizations and deaths typically lag infections by one to three weeks, meaning today’s numbers reflect transmission that occurred earlier in the winter. That lag is one of the key reasons health officials remain concerned even when week-to-week indicators fluctuate.
Long-term care facilities have been especially hard hit, underscoring the vulnerability of older adults and people with underlying health conditions. MDH has emphasized that influenza surveillance now captures hospitalizations statewide, providing a clearer picture of how pressure on hospitals extends well beyond the Twin Cities metro area.

Nationally, the Centers for Disease Control and Prevention (CDC) describes the current season as moderate overall, but with high severity in children and substantial strain on hospitals in multiple regions. As of mid-January 2026, CDC estimates indicate:
What has startled epidemiologists is not just the scale, but the timing. Unlike last year’s flu season, which began early in October, this season stayed relatively muted until mid-December. Then came what some public health experts have called a “switch” effect: doctor visits for flu-like illness surged rapidly in the final weeks of December, reaching their highest weekly levels since 2005 in national outpatient surveillance.
The dominant virus this year is Influenza A (H3N2), a subtype historically associated with more severe seasons. H3N2 infections are more likely than other strains to result in hospitalization, particularly among older adults and young children.
Complicating matters further is the emergence of a newer H3N2 subclade, sometimes referred to in scientific reporting as Subclade K, which began circulating after the 2025–2026 vaccine strains were finalized. Public health researchers say mutations in this subclade allow it to partially evade immunity from prior infection or vaccination.
That reality has fueled understandable anxiety, but officials stress an important nuance: a vaccine mismatch does not mean vaccine failure. CDC analyses consistently show that even in mismatched years, flu vaccination significantly reduces the risk of severe disease, intensive care admission, and death.
One of the most sobering features of this season has been its impact on children. CDC tracking shows record or near-record pediatric hospitalization rates in several states, with dozens of pediatric flu-associated deaths reported nationwide by mid-January. The majority of those deaths occurred in children who were not fully vaccinated.
Older adults remain at the highest overall risk of severe complications, particularly pneumonia and worsening of chronic conditions such as heart and lung disease. Minnesota’s long-term care outbreaks mirror national trends, highlighting how quickly influenza can move through congregate living settings once introduced.
Geographically, the flu’s center of gravity has shifted over time. The Northeast and parts of the South experienced the earliest spikes, with states like New York reporting record-breaking weekly hospitalizations in late December. Activity in the Midwest and on the West Coast has remained stable or increasing through January, suggesting the peak may still be migrating westward rather than fully passing.
That pattern aligns with CDC guidance cautioning against declaring an early peak. Historically, flu seasons often crest between December and February, but timing varies widely, and secondary surges are not uncommon.
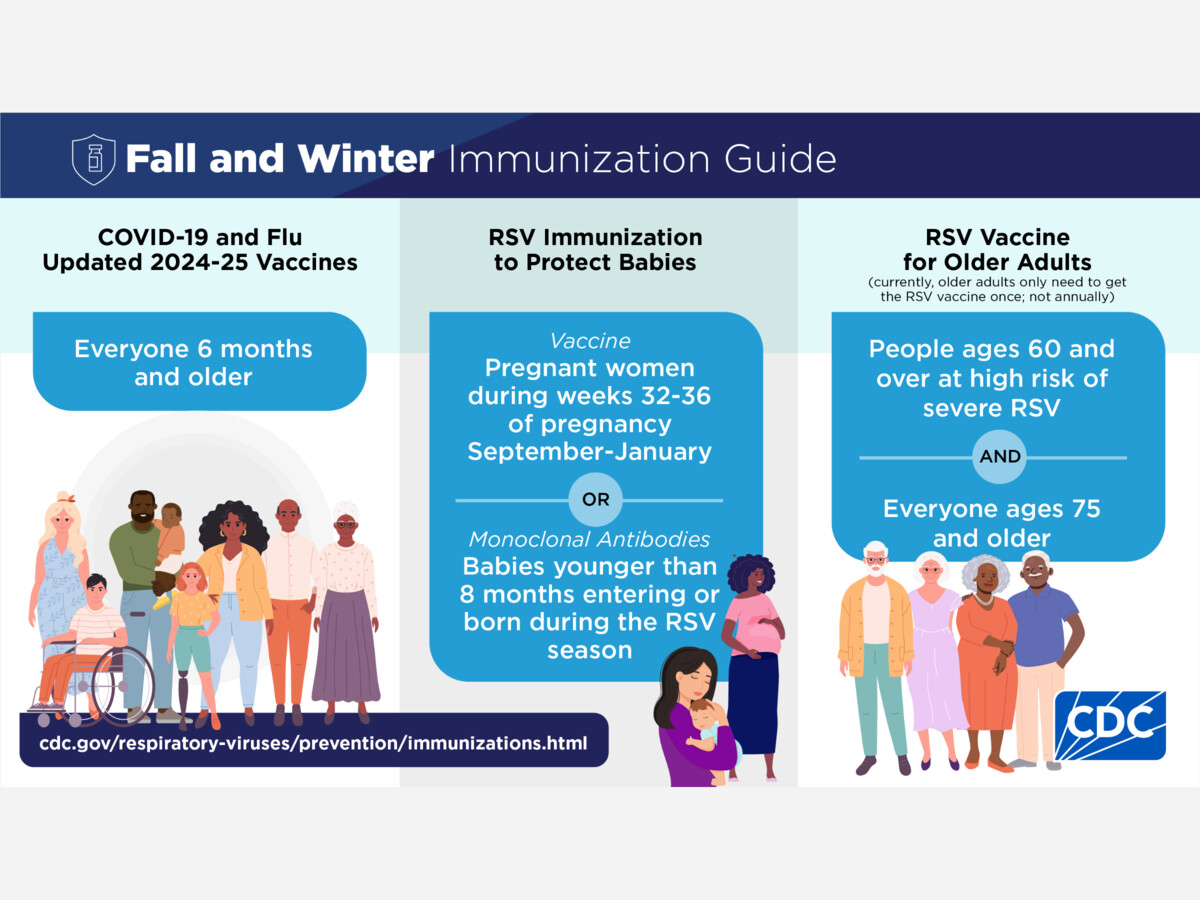
Despite fatigue from years of overlapping respiratory threats, health officials say the guidance remains straightforward and urgent:
Last winter offered a stark reminder of how quickly influenza can accumulate its toll. Minnesota’s 2024–2025 season ultimately produced thousands of hospitalizations and hundreds of deaths statewide, a burden that only became fully visible after the peak had passed.
This year’s trajectory, with severe outcomes still climbing in late January, has public health leaders watching closely. The data so far tell a clear story: the flu season of 2025–2026 is unusual, aggressive, and unfinished. For Minnesota and much of the nation, the weeks ahead remain critical.